2025 AEP and Beyond
As Medicare Advantage continues to evolve under mounting pressures, leaders are strategizing across departments to ensure success in the coming years. Two common themes I have been hearing in my conversations with Drips clients and prospects are adaptability and retention.
Your teams are likely finalizing the details of the 2025 AEP. As I engage with sales, marketing, and CX leaders focused on improving the enrollment experience, I am hearing things like, “We have a renewed focus on retention” or “there is value in keeping our current members engaged.”
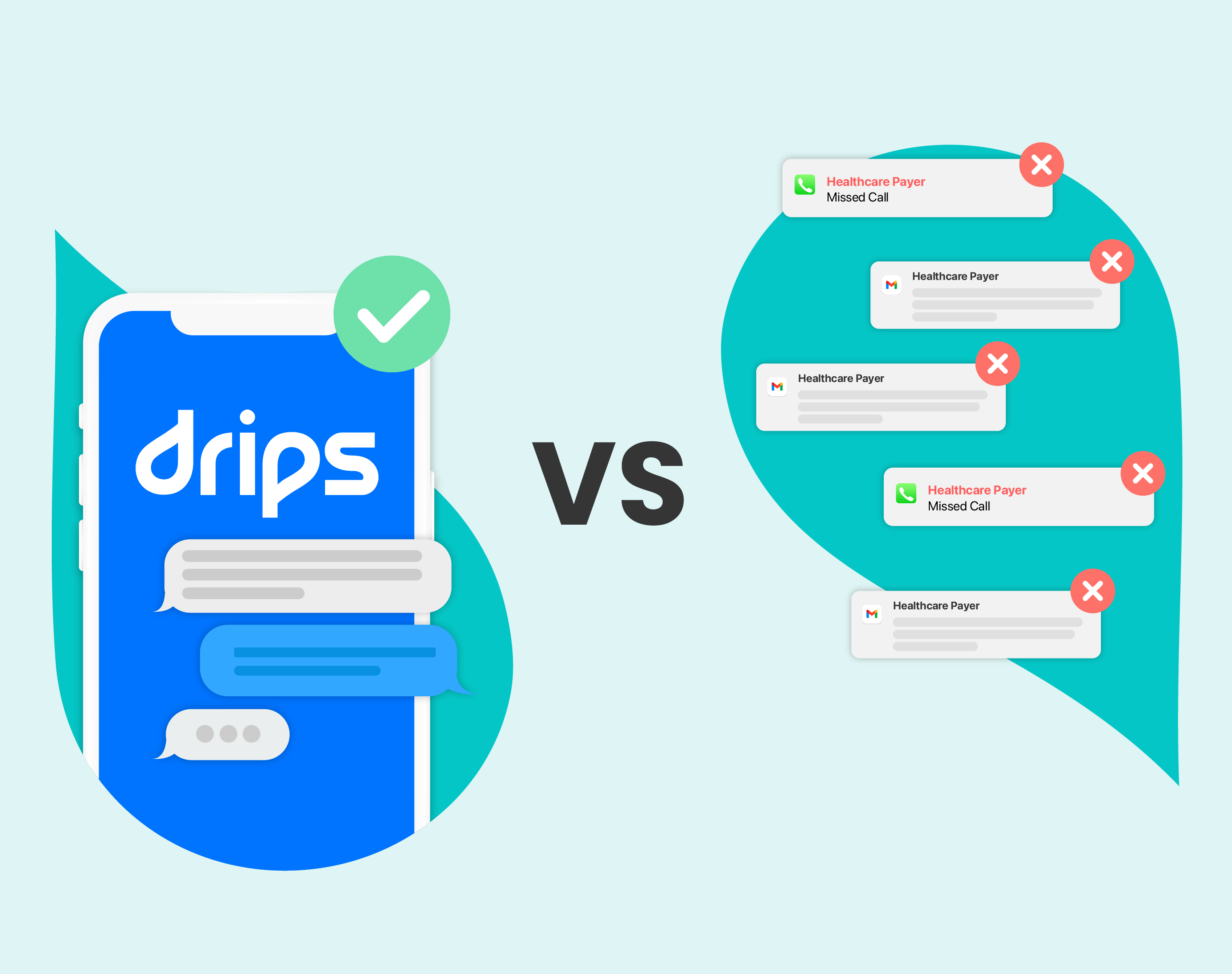
The current CX landscape that healthcare payers have to navigate is complex:
- It's still more costly to acquire new members.
- Maintaining high-quality, compliant outreach is riskier than ever.
- The market is more crowded and noisy.
- Investments in digital initiatives aren't yielding expected returns.
In light of these challenges and considering your organization may be feeling the crunch-time grind, here are three Drips programs in the works for the 2025 AEP and beyond that I’m most excited about. They may inspire some bright ideas for your strategies.
Retain: Member Nurture
Successful organizations regularly engage with their existing members to nurture relationships, understand their needs, and close gaps in care. If you haven't been nurturing these relationships throughout the year, now might be a Hail Mary effort. However, it’s certainly worth considering post-enrollment. Building a trusted relationship through regular, meaningful interactions can significantly enhance member retention.
Retain: Coverage Reviews
Proactively reaching out to existing members during critical times, such as when they receive their Annual Notice of Change or upcoming formulary changes, is crucial. If direct contact is challenging, explore alternative options to engage them. Segmenting members and tailoring messages to their specific needs can help prioritize efforts and ignite relationships. If these discussions aren’t happening today, consider implementing a way to directly engage with members this year or developing a more robust communication strategy to prevent misinformed decisions.
Acquire: Webform Conversions
While many Medicare Advantage-eligible individuals may not be digitally fluent enough to have all their questions answered online, the plethora of available resources has driven traffic to online forms like information requests. Focus on effective follow-up with these potential members, providing space for interested shoppers to mature into live calls when requested. Given the nuanced nature of coverage needs, keep your forms simple, clear, and compliant. Inform members who will contact them and how, based on their preferences.
By addressing these areas, you can improve member retention, enhance engagement, and optimize your enrollment processes for the 2025 AEP and beyond. Adaptability and proactive communication to your members will continue to be a core tenet of driving trust and outcomes, no matter the changes ahead.