Best Practices For A Medicare Advantage Outreach Strategy
When it comes to communicating the complexities of Medicare Advantage, many healthcare insurance providers and brokers are missing the mark when trying to reach seniors. This is a sentiment Kathleen Ellmore, Co-Founder and Managing Director of Engagys, definitely agrees with:
“In this time of uncertainty, getting through the noise — especially health-related noise — has been a challenge. Call centers are a costly option for health plans. A multi-channel approach combining SMS text with call centers has proven to be a great way for the plans we have worked with to boost engagement while keeping outreach budgets in check.” (Engagys)
For seniors, it’s gotten even more difficult for them to trust traditional outreach approaches as they have been the victims of many deceiving business practices. So, it’s a bit of an understatement to say that an adjustment in messaging is clearly needed to earn their trust. Here are some best practice outreach strategies to implement when communicating with seniors.
Don’t Overlook Texting

The stereotype that seniors don’t text is no longer true. According to AARP, 86% of Americans over age 50 communicate regularly via text messaging, and those in the 50-69 age group prefer texting more than email (AARP). The same study also found that those in their sixties were more likely to manage their medical care on smartphones and tablets.
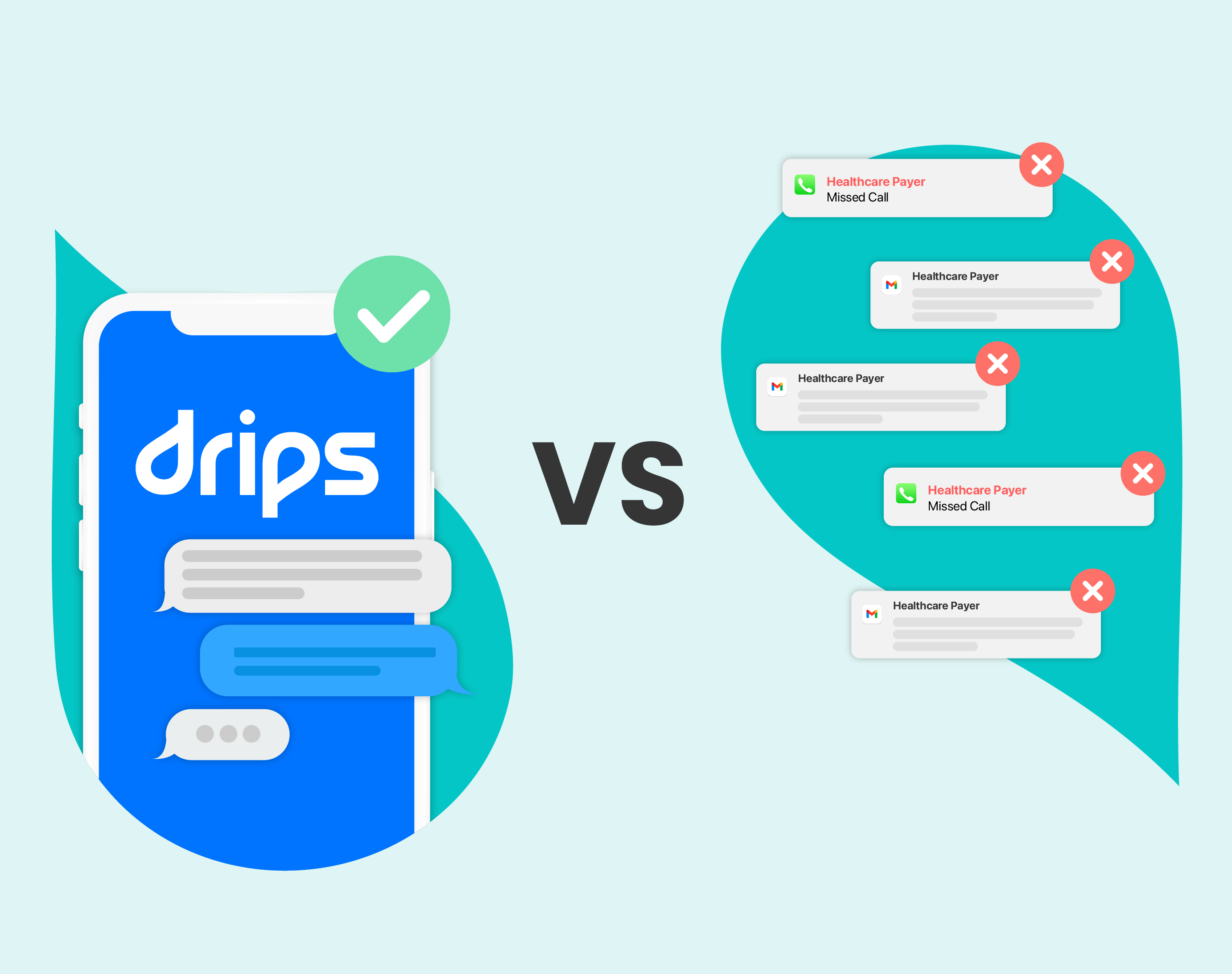
Medicare Advantage marketing efforts that do not use text messages to communicate with their seniors are missing out on an opportunity to communicate efficiently. And those using email or direct mail might find that their messages aren’t being received at all, with email getting an average response rate of 0.6% and direct mail only getting 2.7% (Postary). But simply texting seniors isn’t necessarily going to solve everything; you need to know how to text.
Know How To Text

To make the best use of your text messages, you need to adjust the voice and tone of your message to match the audience. For example, if you tend to use more words or characters in your SMS messages, make sure you account for screen space when the text size on the phone is increased. A longer message might be challenging to read if it involves a lot of scrolling.
This may go without saying, but you should also avoid using emojis in your communications with seniors, as 61% of seniors prefer to engage with messages that don't feature emoticons (Journal of Rehabilitation and Assistive Technologies Engineering). Likewise, you might consider making sure your texts are optimized for text-to-speech and that words are spelled out rather than abbreviated. That way, you'll eliminate confusion and reduce the back and forth asking for clarification. This gives you an opportunity to educate and help seniors through a comfortable medium — it’s a relationship that just isn’t possible with direct mail, or even email.
Expect A Response

Speaking of back and forth, if you’re using SMS to reach seniors about something as technical as Medicare Advantage, you should definitely expect a response to your text and be prepared to answer questions. According to Luma Health, 56% of patients ages 65-84 and even 54% of those ages 85-94 text back to health-related reminders (Luma Health). That’s more often than younger generations respond to similar texts (which is only 49%)!
Also, because large portions of older adults are retired, you'll probably be receiving longer (and more frequent) texts from seniors. This might be a shift from expecting irregular or infrequent responses and may warrant an increase in staff or an alternative method to engage with these additional messages (like an AI-powered conversational outreach strategy that includes SMS).
Partner With Conversational Outreach Professionals

If you’re wondering what these best practices look like in action, we have a case study from our own experience. A top-five health insurance provider wanted to decrease the number of Medicare Part D (prescription drug plan) policy terminations they get from missed payments. They recognized the urgent trouble this could cause policyholders who depend on this coverage and could potentially be priced out of getting the medication they need.
Drips used personalized messaging leveraging our own best practices to either request that policyholders update their account information to avoid losing coverage or to indicate how urgent it was to act immediately (depending on which situation was more appropriate). While primarily SMS-centered, Drips would also direct policyholders to a phone call with a health insurance agent if requested.
In just one month, the health insurer experienced a 290% increase in policy retention. With a larger pool of members the following month, there was a 170% increase in retention compared to the health insurer's existing contact methods and saved more than 3,000 Medicare members from having their policies terminated.
Contact Drips to see how we can help you integrate these best practices into your existing outreach strategy.