How A Top-Five Healthcare Payer Reduced Member Terminations By 39%
A Top-Five Healthcare Payer
A top-five health insurance provider recognized that missed payments could be problematic for members who depend on Medicare Part D coverage. The overall goal was to decrease disenrollments while ensuring members could continue to access the medication they need. This could ultimately improve member health outcomes.
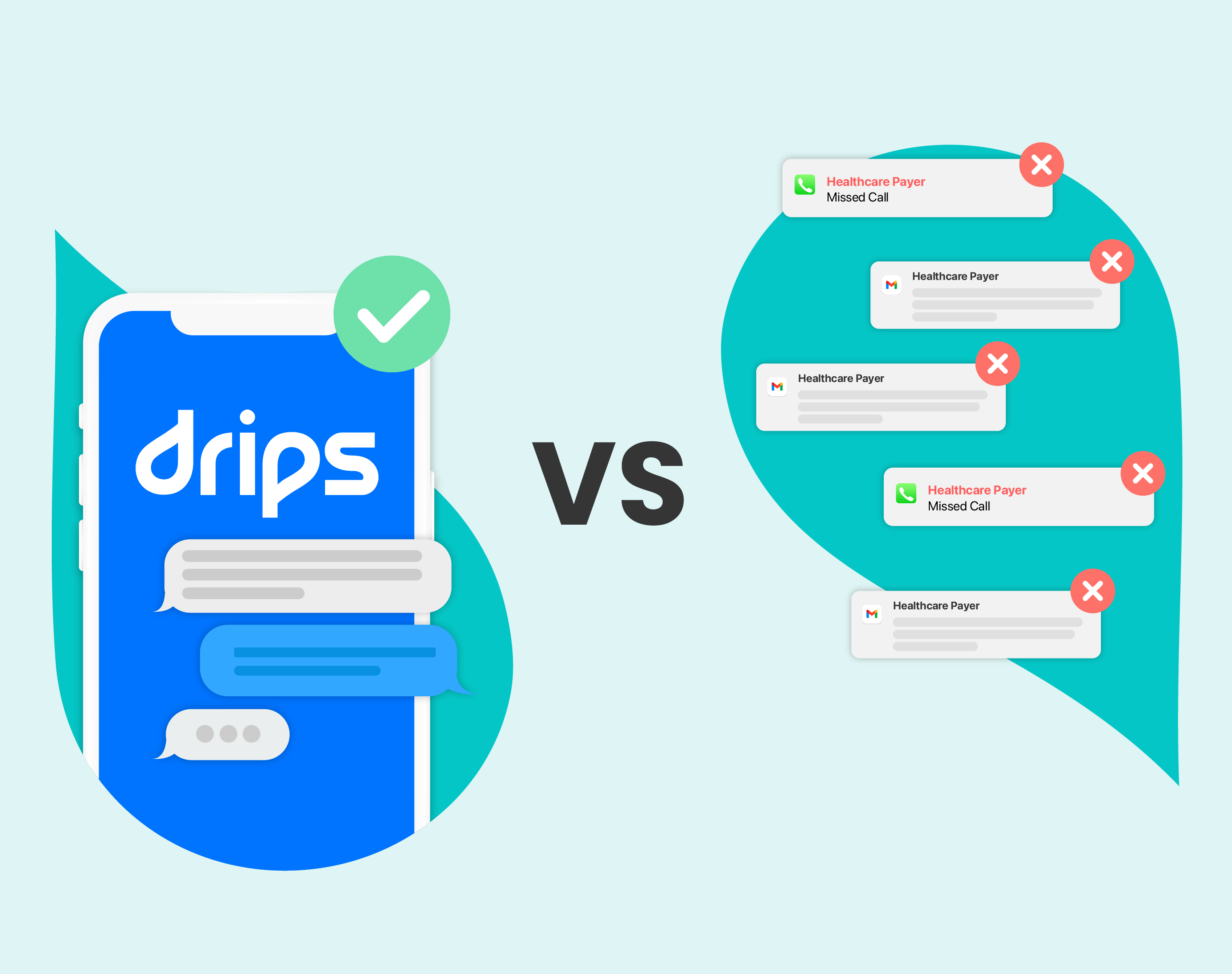
Before Drips
Like most outreach with members today, this payer’s existing outreach method consisted of outbound calls and direct mail campaigns. Unfortunately, they found member engagement was decreasing. As a result, thousands of Medicare Part D policies were terminated every month, with no option for those affected to re-enroll until the next enrollment period or a qualifying life event.
This drove the payer’s Prescription Drug Plan (PDP) team to assess their options for additional outreach. They began looking for a partner to help improve retention, reduce disenrollments, and drive engagement at scale. The payer also aimed to improve the overall member experience as they communicated with an ever-changing population of tech-savvy seniors.
Solution: A Conversational Outbound Strategy
Drips launched coordinated AI-powered conversational outreach campaigns to address multiple points in the retention lifecycle. For bill payment reminders, we sent personalized SMS outreach depending on whether a member was a registered portal user and whether they had been submitted for reminders repeatedly. These individualized messages engaged members and drove them to submit payment online or speak to an agent to complete payment.
Drips also contacted members who had already missed their payment. We used SMS to help engage these members and direct them to a phone call to address payment, or to a custom portal link if they were a registered user. The SMS scripting took an empathy-first approach to meet members where they were and provide helpful guidance about payment options to maintain their drug coverage.
Results: Reduced Terminations
By boosting engagement at multiple points in the funnel, Drips delivered a compounding positive effect for Medicare Part D retention. When the payer compared their actual policy terminations with the expected amount, they found that Drips enabled them to reduce overall terminations by 39%. The payer protected over $8.1 million in revenue from memberships saved with Drips, constituting a 33x ROI from Drips’ conversational strategy. Importantly, each saved membership represented an individual who kept their prescription drug coverage, which is crucial for their health.
In addition, the policy holders contacted through the Drips AI powered platform reported a more pleasant customer experience.






%20Outreach%20Success%20Story-Thumbnail.png)