Health Insurance Company Improves Medication Adherence with a 200% Increase in Refill Rates
Drips Conversations as a Service helped a large health insurance organization improve medication adherence rates for a non-adherent population.
Challenge
A large health insurance company consistently had members who had missed their prescription refills during the previous one to two months. They wanted to support members who had missed their last refill in an effort to improve adherence rates.
Solution
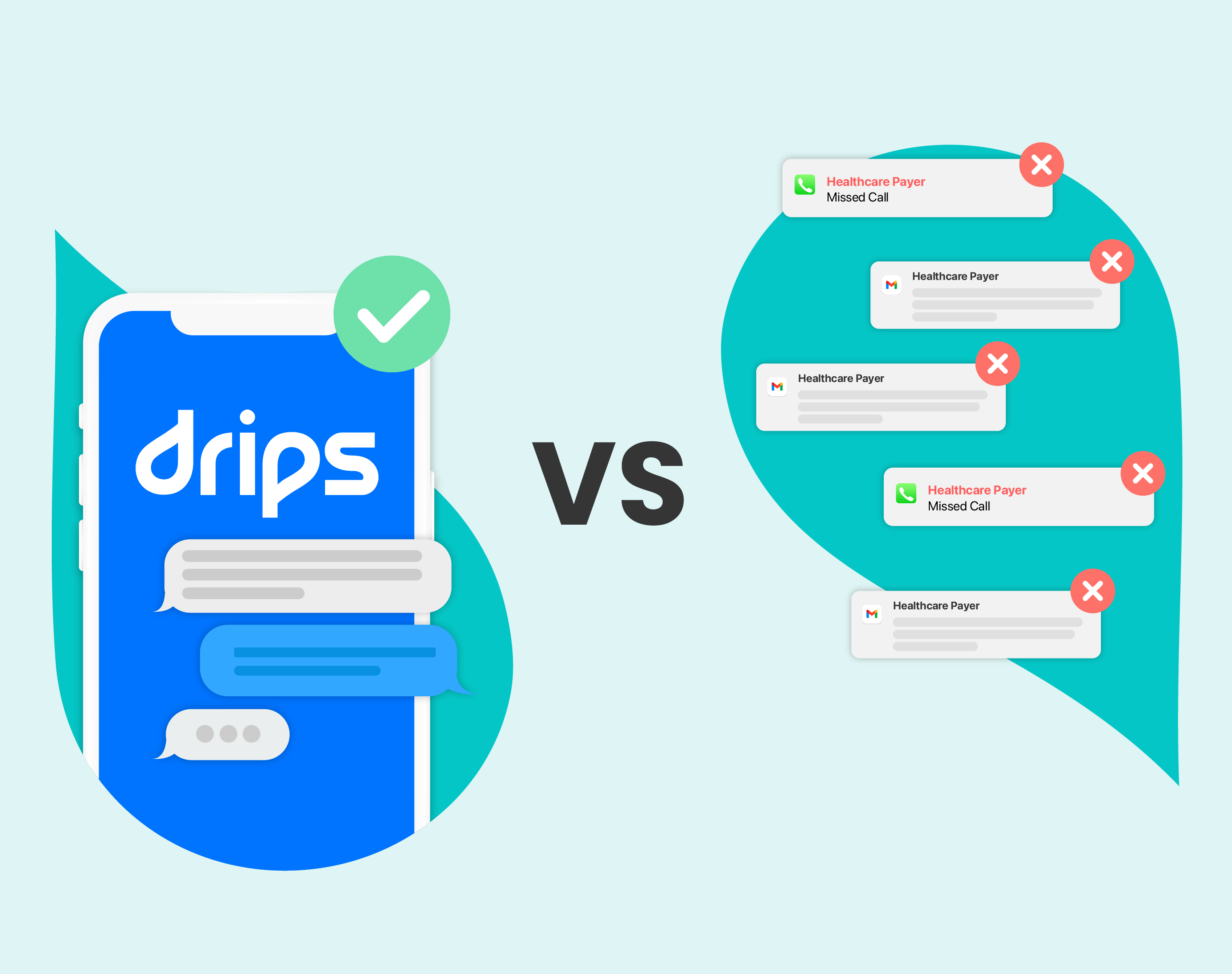
Using Drips Conversations as a Service, the payer was able to engage more effectively with their non-adherent members than previous methods of outbound calling. The goal was to reach a proportion of days covered (PDC) of 80% by the end of the year.
Results
In three months, Drips helped this payer achieve a 200% increase in refill rates when compared to outbound calling outreach.



learn more
Related Resources
learn more
Related Resources
Outreach Insights: Best Practices
Outreach Insights: Best Practices
Case Studies: Healthcare
Case Studies: Healthcare