How a Healthcare Payer Exceeded Their Redetermination Goal by 31%
Drips Conversations as a Service helped a state Blue Cross organization that serves more than 230,000 Medicaid members to significantly improve member engagement and eligibility redeterminations.
Challenge
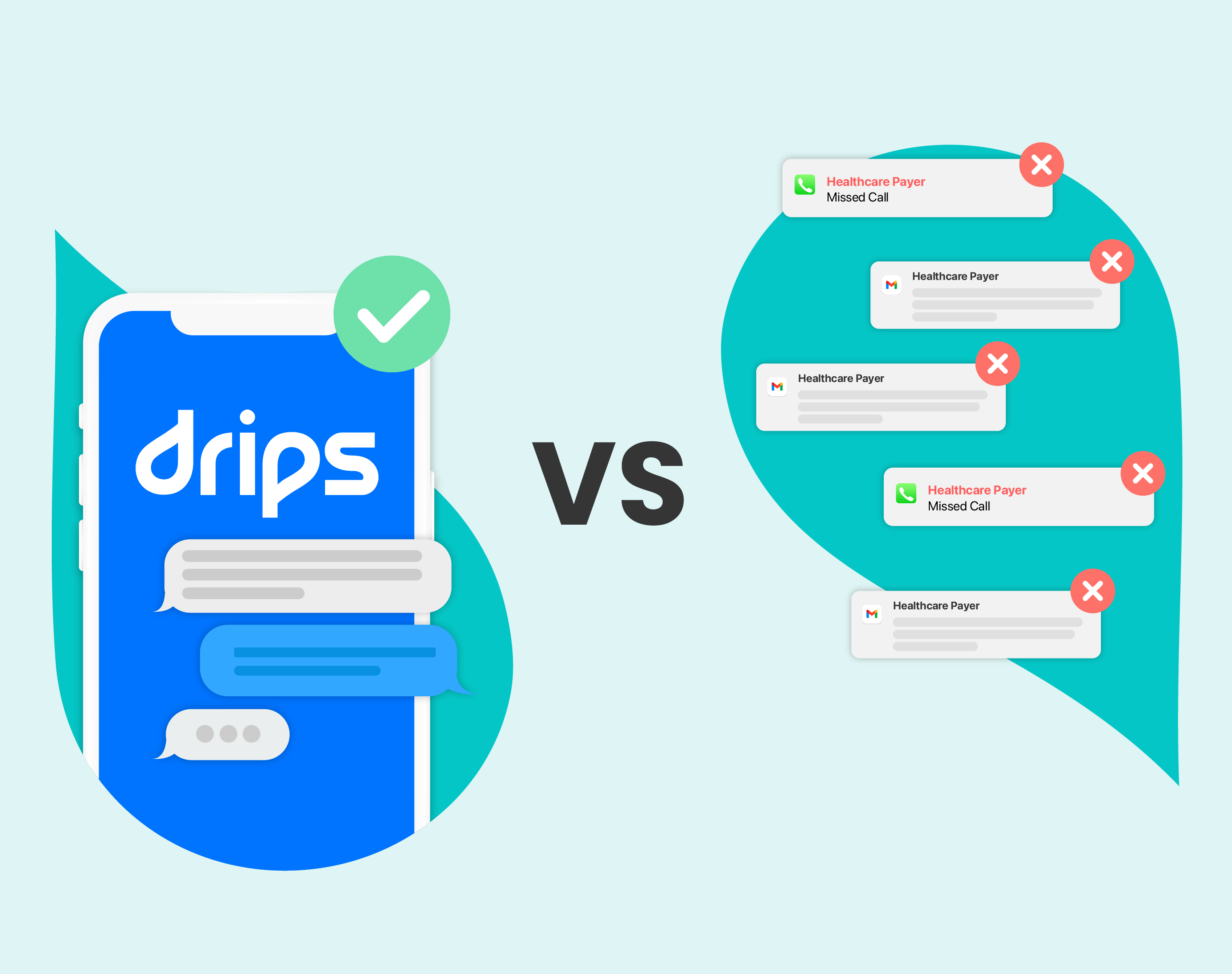
After the end of the COVID-19 Public Health Emergency, this payer struggled to reach members that needed to renew their eligibility for Medicaid. Despite using phone, email, mail, and one-way texts, their connection rate was only 4%.
Solution
Drips' two-way conversational texting approach made it easier for members to engage. Within weeks, their engagement rate jumped from 4% to 40%, connecting with members who otherwise wouldn’t have engaged.

Results
Drips achieved a 10x increase in member engagement and a 31% higher redetermination rate than the payer’s stretch goal, resulting in thousands of members retaining coverage.



learn more
Related Resources
Case Studies: Healthcare
Case Studies: Healthcare
Healthcare: Medicare and Medicaid
Healthcare: Medicare and Medicaid




%20Outreach%20Success%20Story-Thumbnail.png)