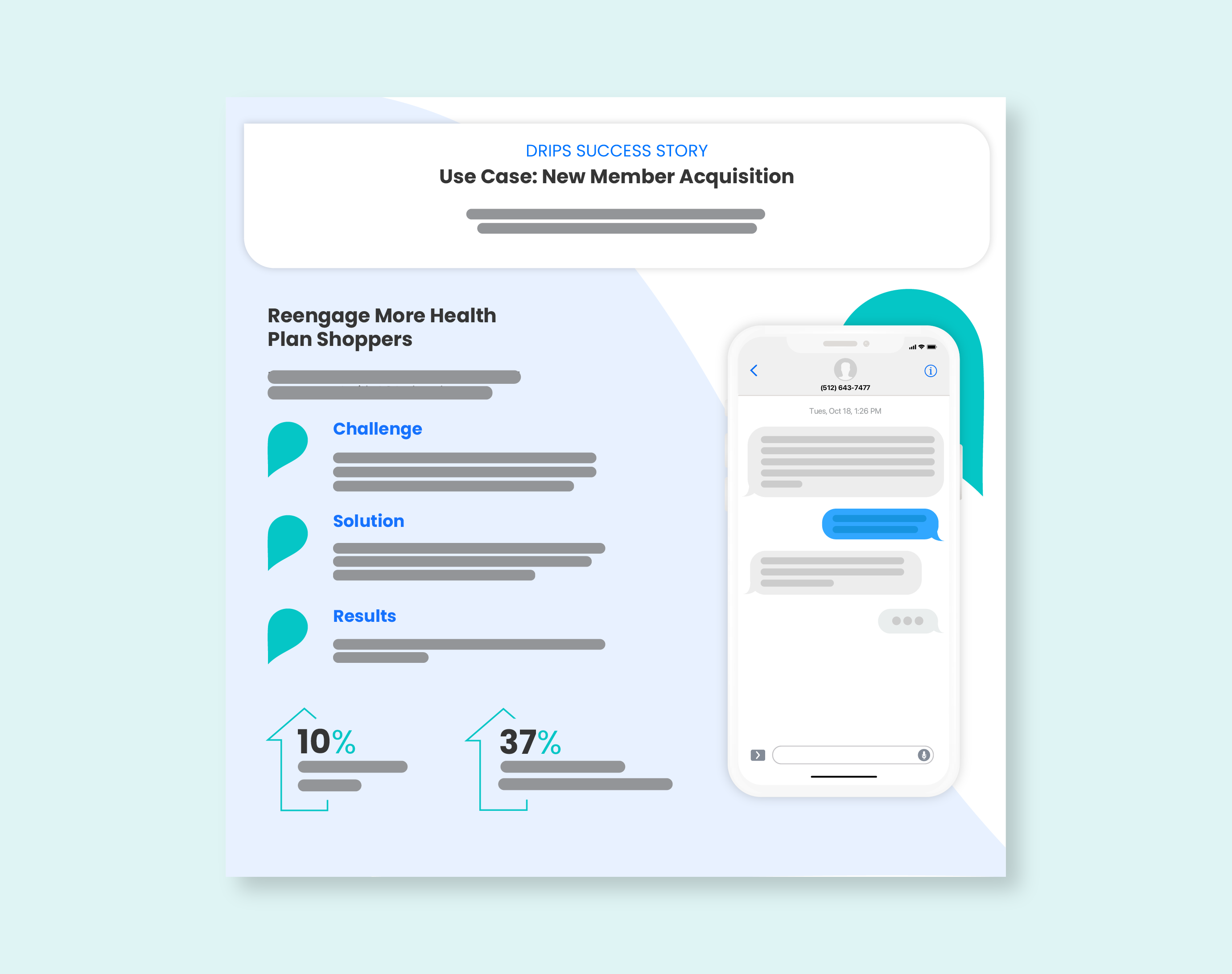
How a Health Payer Improved Member Retention and Satisfaction
Use Case: New Member Acquisition
Seamlessly guide prospective members to digital enrollments or live agent assistance to start or finish enrolling in coverage.
Challenge
A major health payer needed a better way to stay connected with ACA plan shoppers who expressed interest in a plan, but ultimately never enrolled. They used traditional outbound calling to capture and convert these eligible members but fell short due to the intrusive nature of an unannounced outreach.
Solution
Conversations as a Service helped flip the script on reaching members in a way that was convenient and easy to respond on their time. This shift in approach allowed agents to reconnect with members more effectively since calls were requested by the member themselves. Since Drips identifies member intent over SMS, agents didn’t have to spend cycles on members who weren’t interested, allowing them to focus on the ones that were.

Results
The Drips approach allowed for more effective use of agent and member time, significantly impacting their inbound call rate and ultimately conversions.





%20Outreach%20Success%20Story-Thumbnail.png)