How A Top-Five Healthcare Payer Reimagined New Member Education
A Need To Innovate
A top-five healthcare payer knew that effective engagement was essential when educating members. The payer wanted to explore how Drips’ conversational approach could enhance their welcome campaigns.
Challenge: Information Overload & Plan Switching
The top-five healthcare payer faced a challenge after introducing new Marketplace (ACA) plans as part of their lower-premium product portfolio. Some members missed out on information about important plan limitations, resulting in complications and dissatisfaction. For example, virtual-only plans and plans requiring referrals proved to not be the best option for some members.
At first, the payer didn’t have an outreach solution to educate new members about these plans. This meant that dissatisfied members faced a rocky path to understanding the limitations of these newly designed benefits. In some cases, this education gap could lead to grievances and disenrollments.
Solution: Roll Out The Welcome Wagon
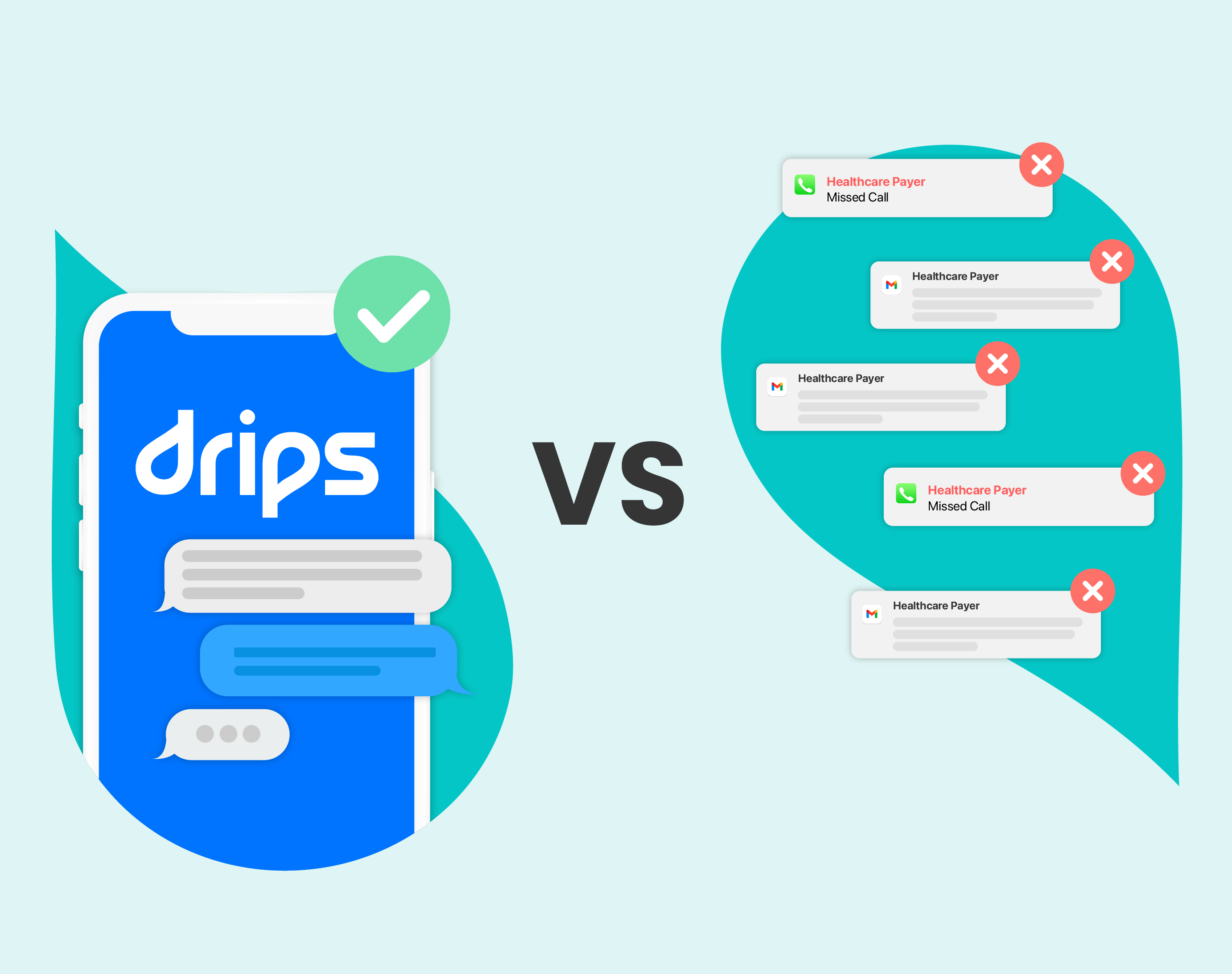
The payer worked with Drips to explore innovative ways to educate new members about their ACA plan benefits. Drips, a leading provider of conversational outreach, uses AI to connect with members through personalized text messages and calls. Whereas traditional methods like outbound dials are increasingly getting ignored by overwhelmed members, conversational outreach excels at engaging members in authentic conversations that lead to measurable outcomes. Especially for younger ACA plan members, creating a genuine connection and using SMS proved to be much more effective than legacy approaches.
With conversational outreach at their disposal, the payer worked with Drips to craft a custom welcome campaign for these ACA members. The campaign checked in on new plan members and answered their questions with carefully crafted and personalized AI responses. If the conversation led to the insight that the member wanted a different plan, Drips helped schedule a call with a licensed agent to ensure the member found another option within the payer’s portfolio.
Results: Helping Members Understand Their Care
The goals of this solution were to improve member education, unearth member pain points, and reduce disenrollments by ensuring members were more satisfied with their plan.
As a result of Drips’ conversational outreach solution, the payer saw a 55% improvement in engagement, compared to a typical response rate for unknown number outbound dials. This engagement meant that these members were getting a better experience and more information about their health plan. At the same time, conversation insights helped the payer understand member pain points before the decision to disenroll, opening an opportunity to educate and retain the member.
In addition, about 2.6% of members contacted decided to switch to a different plan from the payer. By more easily finding the right plan for their needs, these members became less likely to disenroll in the future, boosting retention rates.





%20Outreach%20Success%20Story-Thumbnail.png)